Pain is a very complex entity. Universally, pain is a warning to your body of threats that may bring your body harm. For example, if you touch a hot stove, your body sends a message very quickly to the brain to pull your hand away in order to avoid damage to the tissues.
Acute pain is very different from chronic pain. Acute pain is typically from a specific injury, such as breaking your arm, and the pain disappears when the tissue damage repairs. However, chronic pain typically starts with an acute episode, but it does not resolve with time or treatment, even if the actual tissue that was damaged seems to be repaired. The difference comes from the fact that ALL pain, whether acute or chronic, must be processed by the brain (central nervous system). The way the brain processed pain is influenced by many different factors. This is called Neural Plasticity.
NEURAL PLASTICITY: is a change in the structure, function and organization of neurons (nerve cells) when they are exposed to new experiences. In a healthy brain, the body can adapt to new experiences well. However, in some people, their brain takes on a maladaptive pattern that triggers abnormal processing of pain, and pain becomes heightened and prolonged.
What that means is that there are many theories as to how acute pain starts to turn into chronic pain; however the common factor with all of these theories is that the chronic change happens IN THE BRAIN, not at the site of injury ! This is called CENTRAL SENSITIZATION.
The scientific explanation is quite complicated, so this is a simplified summary of the theory:
Remember it is the nerve cells in the brain that receive the pain input from the injured tissue. In normal nerve cells, the input stimulates the cell and then there is a normal output of the quantity of pain.
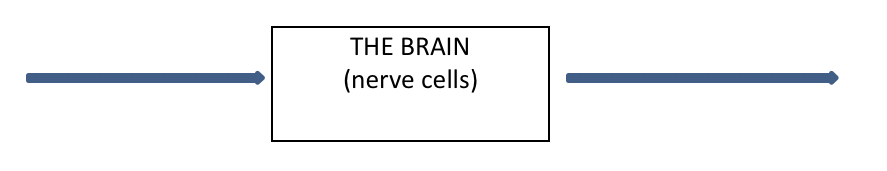
| Input (pain signal from injured tissue) |
Output (“normal” amount of firing & pain perceived) = pain just at the injured tissue |
However, in someone who has chronic pain, the nerve cells have become damaged or more sensitized, and the output from the nerve cells becomes amplified.
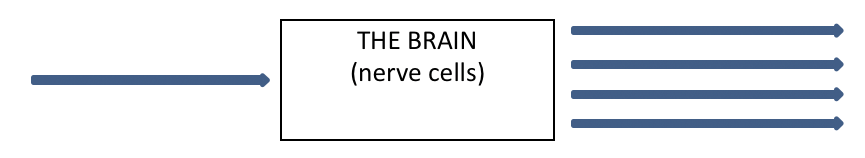
| Input (pain signal from injured tissue) |
Output (“abnormal” amount of firing & pain perceived) = excessive pain with normal touch or activity even in other parts of the body away from the initial injury |
WHY DOES THIS HAPPEN?
Not everyone gets all of the symptoms listed above when their nerve cells start to fire abnormally with chronic pain, but what is consistent is that typically many of the symptoms are not related to the initial injury or pain generating tissue. Some of the more common diagnoses that now include a diagnosis of central sensitization include chronic whiplash disorder, fibromyalgia & chronic fatigue syndrome.
Other related diagnoses that cause acute recurring pain, such as low back pain or headaches or TMJ syndrome, or even tennis elbow can become chronic. Over time, if the problem keeps recurring, it is because the brain has gradually changed to become more sensitized and the postural coping mechanisms that you always used when your back was sore become less and less effective, so acute episodes take longer and longer to heal and then eventually the pain becomes chronic and unrelenting and may “spread” to other areas of the body.
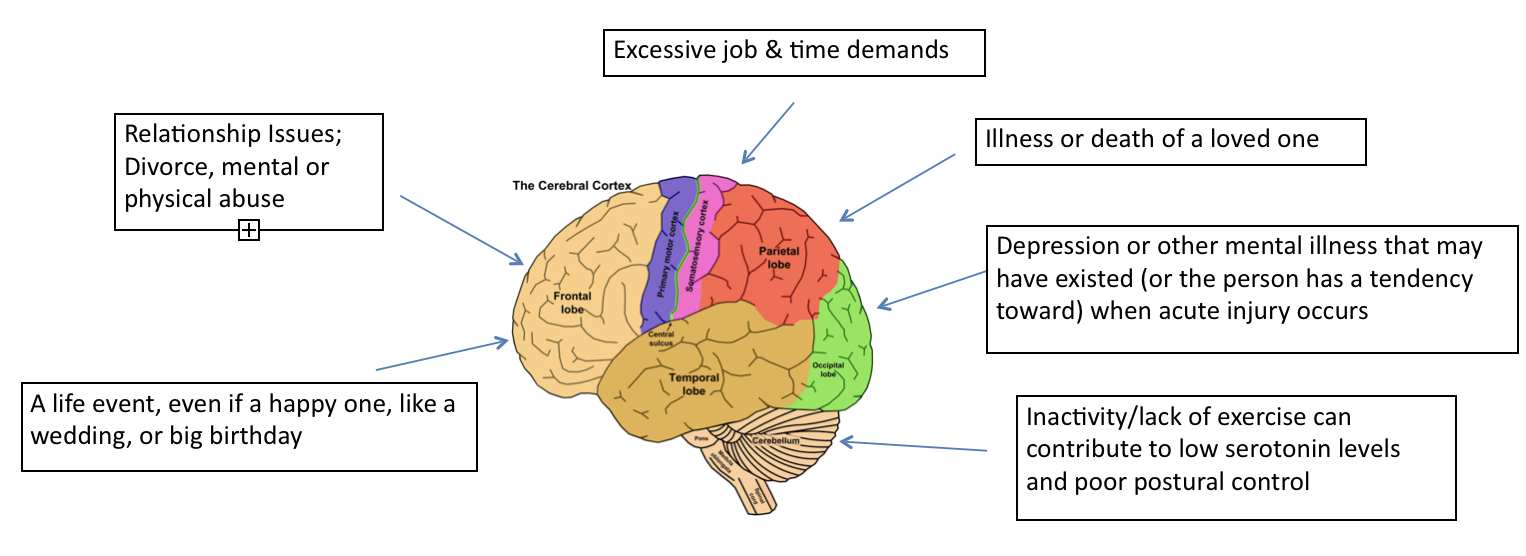
What is also known is that the inability to filter other stress factors, both emotional and physical, affect the nerve cells and becomes another way that the brain becomes sensitized and causes the pain signals to become amplified.
WHAT IS THE TREATMENT ?
Traditional treatment typically involves investigation and treatment at the injury site ONLY. And, as anyone with chronic pain knows, these therapies, such as massage or physiotherapy and even chiropractic care can cause more pain because of the amplified pain signals from just normal touch and movement. The medical solution has been to prescribe pain killers and anti-depressants, which can be helpful to dampen the output of pain signals. However, the drugs create dependency and can also create chemical imbalances, essentially worsening symptoms over the long term.
Therefore, treatment must include therapies that are not only going to treat the original injured tissue, if possible, but it must also address the chronic nerve cell changes that have happened in the brain, by creating different input to the brain.
POSSIBLE SOLUTIONS:
Unfortunately, because everyone is different, their response to treatment will be different, and each person must find what works for them. Here are some ideas and their rationale:
- Exercise: Exercise is paramount and found to be of great benefit in the research. Although exercise will initially be painful, research suggests a “time-contigent” approach, not a “stop when it hurts” approach. What this means is to perform an exercise for 5 minutes regardless of pain. The exercise must be appropriate for what you can do, like swimming or walking or just marching on the spot. The idea is to push through the pain, as research has shown that this helps to deactivate the pain enhancing pathways by making a change. Once you can easily achieve the 5 minutes, then you gradually add a minute at a time.
- Specialized & Specific Chiropractic Care: While chiropractic care is proven very effective in acute low back and neck pain, we still struggle with chronic pain, along with other health care providers. However, recent research is showing that joint stimulation with chiropractic adjustments (not just joint mobilization/movement – there is a big difference!). Most specifically, it is the cerebellum of the brain (see above diagram) that receives the most input from a chiropractic adjustment, especially when the occiput or skull bone is adjusted, as it is the closest bone to the cerebellum. The cerebellum is also what receives input from all joint movement, which is why exercise (and full body adjustments) can be a crucial step to recovery. More research is needed, but Dr. Trim and colleagues trained in specifically adjusting the occiput and upper neck vertebrae, have seen very promising and amazing results with many people. Once an initial change is made, then correction and exercises for the postural system are paramount to help with motor control and continue the healing. This would involve physiotherapy to add exercises that strengthen the postural system.
- Nutrition: This area is poorly researched, but there is certainly lots of anecdotal evidence to show that fixing nutritional and hormonal imbalances in the body will help it heal and can be the change of input that the body needs. Professional help from a holistic nutritionist is the best way to approach this.
- Medications, Nerve Block injections, medical marijuana, etc: As mentioned above, the medications of choice tend to be muscle relaxants, anti-depressants and pain killers, all of which carry many long term side effects. Nerve blocks for painful tissues can be very effective, and provide short term relief. However, they must continue to be administered on a regular basis by a medical doctor specializing in this. Our Clinic, has an excellent referral for this mode of treatment right in the same plaza! Medical marijuana and cannabis oil is a growing field of relief from chronic pain. However, because it cannot be regulated as a drug, research is not extensive. Medical doctors are starting to prescribe this method of pain relief and hopefully it will be studied in more depth soon with reputable clinics providing a good source of product.
If you have more questions about your pain and what might help you, I am happy to discuss the best way to approach your recovery. I am also happy to suggest other referrals to appropriate health care professionals when warranted. If you would like to see some of the research associated with this article, you are more than welcome to see it!

